Clinical Rotations
Prerequisites: Please address in cover letter
- Applicants interested in the Neuropsychology Major Rotation must have sufficient practicum experience (e.g., at least two practicum experiences in neuropsychological/psychological assessment) and have demonstrated familiarity and skills with basic neuropsychological assessment batteries. Two comprehensive neuropsychological evaluation reports, redacted, must accompany the application.
- Prior to being allowed to complete a major CTSCA rotation, interested interns are required to have completed a graduate-level course in developmental psychopathology, and complete a rotation specific interview with the training faculty, as well as online TF-CBT training at https://tfcbt2.musc.edu.
- All applicants considering any rotation are expected to have general coursework and practicum experience in the areas of comprehensive diagnostic evaluation and psychotherapy with individual, couples, family or group.
Major rotations (each 6 months)
Supervisors: Anthony Mannarino, Ph.D., Alvaro Q. Barriga, Ph.D, and Ashley Dandridge, Ph.D.
The Center for Traumatic Stress for Children and Adolescents (CTSCA) is a specialty clinical-research program for children, adolescents, and their families who have experienced traumatic life events. Interns completing a major rotation through CTSCA will receive training in evaluating traumatized children, as well as training in two treatments that have been developed at the Center: Trauma-Focused Cognitive Behavioral Therapy and CBT for Children with Traumatic Grief.
Interns that choose a major rotation through CTSCA will be given the opportunity to provide therapy to patients between the ages of 3 and 18 who have experienced some type of trauma, including, but not limited to, sexual abuse, physical abuse, the traumatic and/or unexpected death of a loved one, natural disaster, and/or serious medical conditions. The intern will ideally carry a caseload of 8-9 clients and will receive one hour of scheduled supervision per week with additional supervision as needed. The CTSCA is extensively engaged in the scientific and empirical development and evaluation of culturally sensitive assessments and intervention with children who have experienced traumatic stress. Faculty provide modeling in the scientist-practitioner approach to clinical activity and interns are encouraged to participate in research, as appropriate, based upon their level of experience and career interest.
Special Prerequisites: Prior to being allowed to complete a major CTSCA rotation, interested interns are required to have completed a graduate-level course in developmental psychopathology, and complete a rotation specific interview with the training faculty, as well as and also the online TF-CBT training at https://tfcbt2.musc.edu.
CTSCA Goals:
- Learn the basic components of assessment with children and adolescents exposed to trauma, including the use of objective instruments to assess trauma symptoms
- Implement Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) with 8-9 cases per week
- Complete TF-CBT, including the trauma narration and processing component, with at least four families
- Use objective instruments to assess treatment outcomes, particularly in regard to PTSD and other trauma symptoms
Adult Trauma-Focused Partial Hospitalization Program
Supervisors: Hilary Rushton, Psy.D. and Sushmitha Mohan, Psy.D.
As part of this rotation, interns obtain experience in the Adult Trauma-Focused Partial Hospitalization Program where they will work with a comprehensive treatment team, including a licensed psychologist, attending psychiatrist, psychiatric residents, psychiatric nurses, and possible psychology graduate practicum students. We serve acute psychiatrically ill adult patients (ages 20+) presenting with a history of trauma, including physical, emotional, interpersonal, sexual, attachment, and medical trauma or other victimization, who are also presenting with severe psychiatric symptoms and mood disorders, including depression, anxiety, OCD, bipolar disorder, personality disorders, and dissociative disorders. This program takes a trauma-informed, integrative approach to stabilization, focusing on applying a trauma-focused lens to all treatment interventions. It uses tenants of evidence-based models, including CBT, DBT, STAIRS, ACT, CPT, mindfulness, and group process interventions, as well as alternative modalities (e.g., expressive therapies). The TF-PHP program serves the Pittsburgh area and treats patients with a range of diverse backgrounds, identities, and clinical concerns.
The intern will gain experience conducting comprehensive biopsychosocial evaluations and facilitating group psychotherapy in a culturally sensitive and affirming manner. Interns gain experience with both skills and process therapy groups. In addition, interns will participate with a multi-disciplinary treatment team and gain an understanding of the interplay between intensive group psychotherapy and assertive medication management of the acutely ill psychiatric patient. As part of the developmental perspective on training, interns will participate in a three stage supervision plan, beginning with observation of the supervisor, co-leading with the supervisor and progression to the supervisor moving to observation of the intern with supervision feedback immediately following the group.
Adult Trauma-Focused Partial Hospitalization Program Goals:
- Observe minimum three process psychotherapy groups
- Plan and lead at least two skills groups
- Plan and co-lead minimum 16 process psychotherapy groups
- Conduct at least two initial evaluations
- Identify and implement minimum of 4 distinct group interventions from CBT, DBT, interpersonal, psychodynamic or other theoretical perspective
- Conduct tiered supervision with practicum students in the program for a minimum of 5 sessions
Neuropsychology
Supervisors: Hollie Dean-Hill, Psy.D., Matthew Page, Ph.D., ABN, Victoria-Maria Sekunda, Psy.D., ABN, Chi Chan, Psy.D.
The 6-month major rotation in neuropsychology is for interns who are pursuing board-eligibility in clinical neuropsychology in order to meet APA Div. 40 Houston Guidelines. This track is for interns with extensive training in neuropsychology prior to internship. Interns who want some exposure to clinical neuropsychology in order to become more well-rounded practitioners are able to complete a year-long minor rotation in neuropsychology. This major rotation will prepare interns for competitive candidacy for neuropsychology post-doctoral fellowship programs. Interns on the advanced track will see a wider variety of clinical cases through both the medical inpatient consult and liaison (C&L) service at Allegheny General Hospital and through the PBHI. Advanced neuropsychology trainees will also be expected to take a more in-depth role with the clinical interview process, test selection, test administration, and report writing consummate with their experience.
The initial stage of the rotation involves careful consideration of the intern’s prior coursework and practicum experiences with standardized assessment more broadly and neuropsychology specifically. Based on the intern’s prior experiences and his/her career objectives for what populations and practice setting he/she desires, an individualized training plan is developed in order to shape the rotation. At different points in training, interns are provided live observation during their training either by neuropsychology post-doctoral fellows and/or faculty members, depending on the supervisor. Interns receive extensive feedback on all aspects of the evaluation process toward preparing the intern for future independent practice.
Hospital Inpatient C&L: Depending on the specific supervisor and the intern’s individual training plan, interns are able to assist with conducting neuropsychological evaluations as part of a consult and liaison (C&L) service for medical inpatients in a level-1 trauma hospital. Approximately 60% of the patients present with traumatic brain injuries, while the remaining cases involve cerebrovascular accidents, hydrocephalus, seizure disorders, pre-/post-surgical evaluations, pre-/post-organ transplant evaluations, medical decision making capacity evaluations, and other acute medical events. These are brief (< 60”) bedside evaluations for acutely ill patients and trains interns in the rapid consult model within an interdisciplinary medical setting.
Outpatient Neuropsychology: All interns will assist with completing comprehensive outpatient neuropsychological evaluations who are referred to the department for a wide-variety of psychiatric and neurocognitive problems, including, but not limited to, traumatic brain injuries (TBIs), cerebrovascular accidents (CVAs), seizure disorders, genetic disorders, progressive neurocognitive disorders, and intellectual disabilities, pervasive developmental disabilities. Depending on the supervisor, interns may gain experience assessing individuals across the lifespan from approximately 6 years of age to 100+ years of age.
Tiered-Supervision: After the intern has demonstrated foundational knowledge and skill in neuropsychological assessment, each intern will provide tiered assessment supervision to graduate practicum students or interns completing the minor rotation in neuropsychology under the ultimate supervision of the intern’s faculty supervisor. This opportunity allows the advanced intern to begin developing and honing his/her own supervisory style in preparing for future independent practice. The intern’s supervision will include a discussion of different supervision theoretical models, the opportunity for role-playing, live observation of the tiered-supervision provided by the intern, and discussion regarding common ethical challenges that can occur in supervisory relationships.
Neuropsychology Rotation Goals:
- The intern will be able to accurately administer and score multiple commonly used, standardized, objective measures from each of the following domains: intellectual functioning, attention, visuospatial and visual-motor construction, language, memory, executive functioning, behavioral and personality functioning.
- The intern will demonstrate a more advanced level of knowledge regarding psychometric theory, including how different normative samples are biased according based sample characteristics, the limits of interpreting data due to either floor or ceiling effects, and the interpretation of a test’s sensitivity and specificity and the relationship these metrics have with diagnostic certainty.
- The intern will be able to assemble neuropsychological test batteries that are appropriate to address common referral questions.
- The intern will be able to fully or nearly entirely complete an initial clinical interview under the direct observation of the supervising Neuropsychologist for a relatively non-complex presenting problem. For more complex referral questions, the intern will be able to conduct most of the interview, particularly the more routine sections of the interview that do not require as specialized or advanced knowledge (e.g., medical history).
- The intern will be able to write a draft of a full neuropsychological evaluation report with appropriate assistance and supervision from the Neuropsychologist.
- The intern will be able to form reasonable diagnostic hypotheses based upon the DSM-5 and ICD-10 criteria for the more straightforward and less complex presenting problems, but is likely to require significant assistance for more complex presenting problems.
- The intern will be able to identify many of the most common ethical dilemmas that arise in Neuropsychology and be able to discuss these dilemmas at a more advanced level in relationship to specific standards outlined in the APA (2002) Ethics Code. The intern should also be familiar with Bush et al.’s (2006) ethical decision making framework in Neuropsychology and demonstrate a rudimentary ability to follow this framework for discussing more complex ethical dilemmas, including being able to identify at least two reasonable courses of action he/she could follow under those hypothetical scenarios.
Yearlong Outpatient Psychotherapy
Adult Outpatient Supervisors: Lori Siegel, Ph.D., Marisa Panucci-Polas, Psy.D., Richard Withers, Ph.D., Sarah Paul, Psy.D., Grace Geidgowd, Ph.D., Sushmitha Mohan, Psy.D., and Julie Pickholtz, Ph.D.
Child Outpatient Supervisors: Richard Withers, Ph.D., Susmitha Mohan, PsyD., and Alvaro Barriga, Ph.D.
As part of the training year, all interns will carry a caseload of at least 4-6 lifespan psychotherapy patients in the outpatient clinic. These cases are part of the intern’s year-long outpatient caseload requirement and serve to ensure the intern has sufficient exposure to a breadth of presenting problems and is able to develop at least basic-level competencies in providing therapy to children, adolescents, and adults.
Adult Outpatient Treatment Goals:
- Intern will identify and work through potential treatment impasses with awareness of the impact of both intern and client variables as measured by successful completion of case presentation/conference.
- Intern will successfully work through the termination process with at least two ongoing psychotherapy cases during the internship year.
- Intern will demonstrate understanding of appropriate referral for ancillary care (e.g., for medication; case management; higher level of care or more specialized care or evaluation), and will learn the processes for making these referrals as demonstrated by at least one appropriate referral during the course of the internship year.
- Intern will demonstrate the ability to develop rapport as evidenced by carrying a case for at least 5 sessions.
Child Outpatient Treatment Goals:
- Demonstrate familiarity with DSM-V/ICDM-10 diagnoses common to children and recognize developmental differences between adult and childhood presentation of common mental health diagnoses.
- Be able to articulate a general knowledge of healthy and problematic child and adolescent psychological development.
- Recognize different engagement and therapeutic communication strategies appropriate to child and adolescent work.
- Be able to articulate basic understanding of agents of change in major evidence-based approaches to child psychotherapy (e.g., Cognitive-Behavioral, Psychodynamic, Child-Centered and family-focused treatments).
- Be able to articulate rudimentary knowledge of parenting skills: behavioral principles, age-appropriate expectations and developmental needs of children of different ages.
Child and Adolescent Assessment
Supervisors: Alyssa Stiver, Psy.D. and Amanda Traficante, Ph.D.
The internship offers a major rotation in psychological assessment through the PBHI for interns seeking to develop expertise in assessing for autism, ADHD, and learning disorders in children and adolescents. During this rotation, interns will gain experience with administering and scoring the Autism Diagnostic Observation Schedule, Second Edition (ADOS-2) under the direct supervision of the supervising psychologist. This training experience is well-suited for interns who would like to specialize in evaluating and diagnosing common childhood disorders, including ADHD, anxiety, and mood-related concerns. This rotation provides specialization in diagnostic evaluation of autism spectrum disorder (ASD) and other neurodevelopmental disorders. In this setting, interns will be exposed to a variety of presenting problems in children ages 6-21 without medical complexity who present for diagnostic assessment. Interns will also gain experience with the administration of other standardized tests that measure intellectual functioning, academic achievement, learning, attention, executive functioning, behavioral functioning, and personality functioning. Interns will also be involved in a 6-week parent management training group for parents of children in kindergarten through fifth grade with ADHD or behavioral disorders. At the completion of the training year, interns will have the skills to complete an initial diagnostic interview, administer objective, standardized assessments, write integrated reports, and communicate diagnostic findings to families.
Prerequisites: Interns must demonstrate previous experience with testing children and adolescents (e.g., competence with administering the WISC-V, WAIS-IV, WIAT-4, and WJ tests). Prior ADOS-2 training and exposure is preferred but not required.
Child and Adolescent Assessment Major Rotation Goals:
- The intern will be able to accurately administer and score multiple commonly used, standardized, objective measures from each of the following domains: intellectual functioning, academic achievement, learning, attention, executive functioning, behavioral, and personality functioning.
- The intern will gradually develop competence with administration and scoring/coding of the Autism Diagnostic Observation Schedule, Second Edition (ADOS-2), under the direct supervision of the supervising psychologist.
- The intern will be able to assemble psychological test batteries that are appropriate to address presenting patient concerns and referral questions.
- The intern will be able to fully or nearly entirely complete an initial clinical interview under the direct observation of the supervising psychologist for a relatively non-complex presenting problem. For more complex referral questions, the intern will be able to conduct most of the interview, with support as-needed from the supervising psychologist.
- The intern will be able to write a draft of a full psychological evaluation report with appropriate assistance and supervision from the supervising psychologist within an agreed upon time frame.
- The intern will be able to form reasonable diagnostic hypotheses based upon the DSM-5 and ICD-10 criteria for the more straightforward and less complex presenting problems, but is likely to require significant assistance for more complex presenting problems.
- The intern will be able to identify many of the most common ethical dilemmas that arise in psychological assessment and be able to discuss these dilemmas at a more advanced level in relationship to specific standards outlined in the APA (2002) Ethics Code.
- The intern will clearly communicate testing results, diagnostic conceptualization, and recommendations to patients and families in a clear, compassionate manner under the direct supervision of the supervising psychologist. The intern will also be able to effectively answer patient/family questions and address concerns.
- The intern will be able to seek out relevant research when more complex cases arise in order to enhance their clinical practice.
- The intern will be able to establish appropriate rapport with patients, implement interventions that are evidence-based and well-timed for the patient, conceptualize cases and develop plans for treatment based on presenting concerns, and make appropriate referrals for patients with support from the licensed psychologist when complex cases arise.
- The intern will be able to effectively collaborate and consult with other professionals by participating in available treatment teams and contacting other professionals on a patient’s care team when appropriate.
- The intern will be able to function effectively as a group facilitator with support from a licensed psychologist. The intern will be able to modify the group content to address patient concerns and discussions in the moment. The intern will understand and implement group interventions focused on parent management training/behavior modification, coping skills, and problem solving skills.
Women's Behavioral Health (WBH)
Supervisors: Miriam Reder, Ph.D., and Katy Cherry, PhD
As part of this rotation, interns obtain experience in individual therapy with women and/or birthing parents and their families who are presenting for treatment of perinatal mood and anxiety disorders, distress related to infertility and perinatal loss. Interns can also obtain experience in evidence based dyadic psychotherapies such as PCIT-Toddler, Parent Child Psychotherapy, and DIRFloortime within our Maternal Infant Health Program. Under the umbrella of Women’s Behavioral Health, this program specializes in treating parent and young children when the parent-child relationship is at risk due to trauma, parental mental health, or other concerns.
In addition, interns will receive training facilitating group psychotherapy with acutely ill women experiencing severe perinatal mood and anxiety disorders in our Mother-Baby Intensive Outpatient Program. The Mother-Baby Intensive Outpatient Program takes an integrative, evidence-based approach to the treatment of perinatal mood and anxiety disorders, including a curriculum of CBT, DBT, BA, and IPT modules and regular practice of mindfulness. The program also incorporates a dyadic curriculum aimed at strengthening the relationship between mother and baby, which includes perinatal yoga, infant sign language, Circle of Security, child development, infant massage, baby wearing, raising emotionally intelligent children, PCIT-Toddler Skills, and PCIT-Toddler skills, and a collaboration with local early intervention services.
The intern will gain experience conducting comprehensive biopsychosocial evaluations, providing evidenced-based treatments to individuals, and facilitating group psychotherapy in a culturally sensitive and affirming manner. In addition, interns will participate with a multi-disciplinary treatment team and gain an understanding of the interplay between intensive group psychotherapy and assertive medication management of the acutely ill psychiatric patient. In addition, the intern will also learn to understand the impact of perinatal mood and anxiety disorders on the entire family and will have an opportunity to participate in family sessions. As part of the developmental perspective on training, interns will participate in a developmental supervision plan while rotating in the Mother-Baby IOP, beginning with observation of the supervisor, co-leading with the supervisor and progression to the supervisor moving to observation of the intern with supervision feedback following the group.
WBH Major Goals:
- Conduct at least six initial evaluations
- Carry a caseload of four to six outpatient therapy patients, at least one of which is enrolled in IOP, as available
- Plan and co-lead at least 12 IOP groups
- Complete at least one family session for an IOP patient
- Identify and implement minimum of 4 distinct group interventions from CBT, DBT, BA, interpersonal, or other theoretical perspective
- Conduct tiered supervision with practicum students in the program for a minimum of 5 sessions, as the opportunity allows
- The intern will participate in weekly multi-disciplinary team meetings.
- The intern will be able to identify some of the common ethical dilemmas that most frequently arise when working with perinatal patients and be able to discuss these dilemmas at an introductory level in relationship to specific standards outlined in the APA (2002) Ethics Code.
- The intern will develop an understanding of the unique clinical features of psychiatric symptoms in a perinatal population and will be able to demonstrate the ability to complete a thorough psychological assessment and case conceptualization with perinatal patients.
- The intern will develop knowledge of empirically supported psychotherapies for perinatal mood and anxiety disorders, including Interpersonal Psychotherapy, Cognitive Behavioral Therapy, Behavioral Activation, and Dialectical Behavior Therapy.
- The intern will be able to demonstrate a working knowledge of cultural considerations related to perinatal patients including recognition of cultural influences of self and others in accessing mental health treatment during the perinatal period.
- Develop and present one hour presentation on perinatal topic to WBH clinical team or develop component of IOP curriculum and present in IOP group.
Minor rotations
Adult Clinical Health Psychology: Minor Rotation
Supervisors: Matthew Iwaniec, Psy.D. and Chelsea Neill, Psy.D.
This rotation is primarily located at West Penn Hospital (WPH) within the AHN Psychiatric and Behavioral Health Institute, although there may be an infrequent need to travel to off-site locations for some clinical experiences (e.g., transplant evaluations at AGH). The primary goal of the rotation is to provide clinical health psychology training within an academic medical setting. Clinical Health Psychology is a specialty that is dedicated to the development of knowledge regarding the interface between behavior and health, and to the delivery of high-quality services based on that knowledge to individuals, families, and health care systems. Interns choosing this minor rotation will have flexibility to choose among the listed training opportunities to find a combination that provides the best fit with their training experiences and career goals.
Training Opportunities
- Delivering behavioral health consultation and liaison services to WPH medical-surgical care units, including Burn, Acute Rehabilitation, Cardiothoracic ICU, Med-Surg ICU, Progressive Care Unit, Hematology and Cellular Therapy, and Medical Oncology.
- Conducting pre-surgical psychological evaluations for bone marrow/cell transplant and CAR-T therapies
- Shadowing and collaborative work with the inpatient Psychiatry C&L service at West Penn
- Shadowing and collaborative work with the Palliative Care service at West Penn
- Training in Empowered Relief for Chronic Pain
- Providing tiered supervision with practicum students
- Developing competencies in effective and appropriate interprofessional communication within a team-based approach to patient care, by participating in weekly multi-disciplinary team meetings
- Developing a comprehensive understanding of pertinent ethical, interprofessional, and administrative issues related to the provision of Clinical Health Psychology services in medical settings
- Participating in delivering group coping skills training to surgical oncology patients
- Developing and presenting a one-hour presentation on a burn injury related topic to our local West Penn burn survivor group, Burn Concern of Western Pennsylvania.
- Conducting program development or quality improvement projects for integrated care teams.
Neuropsychology: Minor Rotation
Supervisors: Hollie Dean-Hill, Psy.D., Matthew Page, Ph.D., ABN, Victoria-Maria Sekunda, Psy.D., ABN, and Chi Chan, Psy.D.
A minor rotation in neuropsychological assessment was developed for interns aiming to be psychologists with more comprehensive diagnostic testing experience. Interns will engage in test selection, administration, interpretation, and report-writing in an outpatient setting, under the supervision of a neuropsychologist. This rotation affords exposure to a variety of neuropsychiatric, neurodevelopmental, and neurocognitive concerns, depending on intern skill, interest, and goals, with a predominant focus on developing assessment and diagnostic skills.
This rotation can be tailored to be specific to child and adolescent assessment if an intern is looking to expand diagnostic and functional assessment of children and adolescents in particular. This can include assessment of intellectual, broad cognitive, academic, behavioral, and emotional functioning in children and adolescents with various questions regarding neurodevelopmental and other common childhood concerns.
Neuropsychology Minor Rotation Goals:
- The intern will be able to accurately administer and score at least one commonly used, standardized, objective measure from each of the following domains: intellectual functioning, attention, memory, executive functioning, and personality functioning.
- The intern will demonstrate a foundational level of knowledge regarding psychometric theory, including how to derive normative scores from raw scores and how to translate between T-score, Z-scores, Standard Scores, Scaled Scores, and percentiles.
- The intern will be able to assist the supervising Neuropsychologist with completing an initial clinical interview and demonstrate how foundational interviewing skills, such as establishing rapport and gathering accurate data, can be applied to patients with complex psychiatric and co-morbid medical histories.
- The intern will be able to write portions of the neuropsychological report (e.g., parts of the background section and behavioral observations), but is likely to require significant assistance and feedback on the following sections: test summary, diagnostic impressions, and the conclusions and recommendations.
- The intern will demonstrate that ability to broadly conceptualize a neuropsychological assessment case by integrating data from the clinical interview, test data, and behavioral rating scales, and to offer some relevant recommendations.
- The intern will be able to identify some of the common ethical dilemmas that most frequently arise in Neuropsychology and be able to discuss these dilemmas at an introductory level in relationship to specific standards outlined in the APA (2002) Ethics Code.
- The intern will be able to demonstrate a working knowledge of cultural considerations related to neuropsychological assessment, including recognition of cultural influences of self and others in the assessment process and strengths and limitations of the assessment process as they related to diversity.
Child Integrative Therapy (12 months)
Supervisor: Richard Withers, Ph.D.
Provides a more in-depth experience in child psychotherapy with a wider exposure to different psychopathology and treatment needs for children, adolescents and their parents. Developmentally informed case-conceptualization and integration of psychodynamic, cognitive-behavioral and child-centered treatment approaches will be encouraged. The minor will include training in evidence-based therapeutic uses of play and art with children and adolescents. Interns will teach behavior-management strategies to parents for challenging behaviors associated with impulse control, mood and anxiety disorders, etc. Interns will also become familiar with more specialized treatment approaches, such as behavioral treatments for anxiety disorders and OCD, and treatment approaches for Autistic Spectrum Disorders. Exposure to and training in these treatments will be provided as cases arise.
Child Integrative Therapy Minor Rotation Competencies:
In addition to general child outpatient therapy competencies, interns would be expected to:
- Demonstrate competency in therapeutic communication with children and adolescents of different ages and developmental levels (be able to converse with children who indicate that they feel understood and understand the clinician).
- Demonstrate competence in at least one evidence-based therapeutic approach to children and adolescents, including:
- Completion of a thorough psychosocial intake.
- Demonstration of ability to engage both children and their parents collaboratively in treatment planning, while maintaining appropriate boundaries and respecting confidentiality.
- Ability to set specific and measurable goals in the form of a treatment plan, appropriate to diagnoses and individual child and family needs.
- Ability to carry out the basic treatment strategies consistent with one or more evidence-based approaches in a manner appropriate to individual children and their families.
- Demonstrate ability to effectively and appropriately communicate with other child service providers, including physicians, educators, social workers and service coordinators.
- Demonstrate a basic understanding of child abuse reporting laws and procedures for handling child and adolescent emergencies.
Women's Behavioral Health: Minor Rotation
Supervisors: Katy Cherry, Ph.D. and Miriam Reder, Ph.D.
This rotation will be located in the AHN Women’s Behavioral Health department, located at West Penn Hospital. The population in this rotation will be perinatal and postpartum patients struggling with infertility or pregnancy loss, perinatal mood and anxiety disorders, perinatal OCD, and/or trauma. Training will include psychiatric assessments, individual psychotherapy with outpatient populations and group psychotherapy in the Mother-Baby Intensive Outpatient Program. Training will incorporate empirically-validated treatments for the perinatal population, including IPT, CBT and behavioral activation, and DBT. The intern will have opportunities for weekly individual supervision and participation in the weekly IOP group supervision/consultation meeting.
Women’s Behavioral Health Minor Rotation Goals:
- Develop an understanding of psychiatric symptoms in a perinatal population
- Demonstrate the ability to complete a thorough psychiatric assessment with perinatal patients
- Develop an understanding of empirically supported psychotherapies for perinatal mood and anxiety disorders including, cognitive behavioral therapy, dialectical behavioral therapy, interpersonal psychotherapy, and behavioral activation.
- Complete individual treatment with two perinatal patients
- Demonstrate ability to co-lead Mother-Baby Intensive
- Outpatient therapy group
- Participation in weekly team meetings
- Develop and present one hour presentation on perinatal topic to WBH clinical team or develop component of IOP curriculum and present in IOP group.
- Participate in one community event to raise awareness of perinatal mood and anxiety disorders
Intern training programs example
The example training programs below are provided for illustrative purposes only and represent just a few of the major and minor rotation combinations available to give the prospective applicant a sense of the wide variety of unique training programs the intern is able to craft.
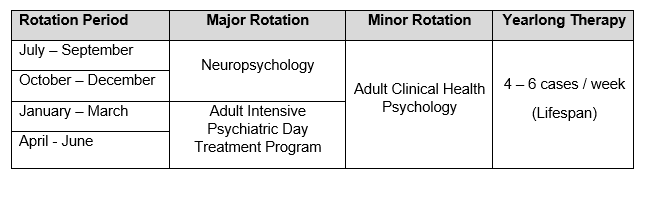
Lifespan treatment
This is a sample training program for an intern interested in gaining a full range of child, adolescent and adult therapy experiences.
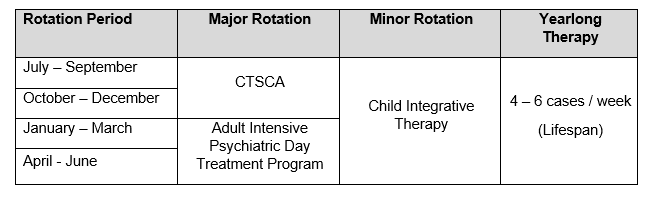
Integrative care treatment
This is a sample training program for an intern who is interested in providing evidenced-based treatment within a medical system, emphasizing providing therapy both for survivors of trauma, and also within an intensive outpatient program designed for perinatal women experiencing psychiatric difficulties.
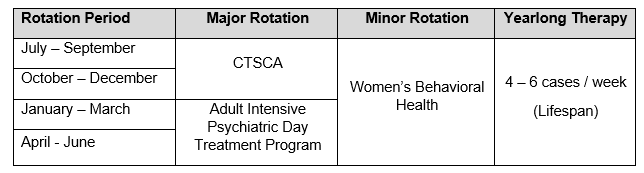
Child Neuropsychology & Treatment-focused
This sample training program would be ideal for the intern who wants in-depth training in child neuropsychological assessment to meet Div. 40 Houston Guidelines, while obtaining additional competencies in CBT therapy with children and adolescents while gaining exposure to pediatric consultations within a children’s hospital.
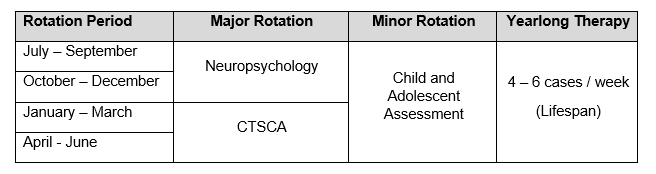
Adult Neuropsychology & Treatment-focused
This sample training plan is designed for the intern who wants advanced training in adult neuropsychological assessment across multiple settings in addition to developing competencies for providing adult psychotherapy within acutely ill psychiatric patients.